Myasthenia gravis
| Myasthenia gravis | |
|---|---|
 | |
| Eye deviation and a drooping eyelid in a person with myasthenia gravis trying to open her eyes | |
| Specialty | Neurology |
| Symptoms | Varying degrees muscle weakness, double vision, drooping eyelids, trouble talking, trouble walking[1] |
| Usual onset | Women under 40, men over 60[1] |
| Duration | Long term[1] |
| Causes | Autoimmune disease[1] |
| Diagnostic method | Blood tests for specific antibodies, edrophonium test, nerve conduction studies[1] |
| Differential diagnosis | Guillain–Barré syndrome, botulism, organophosphate poisoning, brainstem stroke,[2] metabolic myopathies |
| Treatment | Medications, surgical removal of the thymus, plasmapheresis[1] |
| Medication | Acetylcholinesterase inhibitors (neostigmine, pyridostigmine), immunosuppressants[1] |
| Frequency | 50 to 200 per million[3][4] |
Myasthenia gravis (MG) is a long-term neuromuscular junction disease that leads to varying degrees of skeletal muscle weakness.[1] The most commonly affected muscles are those of the eyes, face, and swallowing.[1][5] It can result in double vision, drooping eyelids, and difficulties in talking and walking.[1] Onset can be sudden.[1] Those affected often have a large thymus or develop a thymoma.[1]
Myasthenia gravis is an autoimmune disease of the neuromuscular junction which results from antibodies that block or destroy nicotinic acetylcholine receptors (AChR) at the junction between the nerve and muscle.[6][7][1] This prevents nerve impulses from triggering muscle contractions.[1] Most cases are due to immunoglobulin G1 (IgG1) and IgG3 antibodies that attack AChR in the postsynaptic membrane, causing complement-mediated damage and muscle weakness.[8] Rarely, an inherited genetic defect in the neuromuscular junction results in a similar condition known as congenital myasthenia.[9][10] Babies of mothers with myasthenia may have symptoms during their first few months of life, known as neonatal myasthenia[1] or more specifically transient neonatal myasthenia gravis.[11] Diagnosis can be supported by blood tests for specific antibodies, the edrophonium test, electromyography (EMG), or a nerve conduction study.[1]
MG is generally treated with medications known as acetylcholinesterase inhibitors, such as neostigmine and pyridostigmine.[1] Immunosuppressants, such as prednisone or azathioprine, may also be used.[1] The surgical removal of the thymus may improve symptoms in certain cases.[1] Plasmapheresis and high-dose intravenous immunoglobulin may be used during sudden flares of the condition.[1] If the breathing muscles become significantly weak, mechanical ventilation may be required.[1] Once intubated acetylcholinesterase inhibitors may be temporarily held to reduce airway secretions.[12]
MG affects 50 to 200 people per million.[3][4] It is newly diagnosed in 3 to 30 people per million each year.[13] Diagnosis has become more common due to increased awareness.[13] MG most commonly occurs in women under the age of 40 and in men over the age of 60.[1][5][14] It is uncommon in children.[1] With treatment, most live to an average life expectancy.[1] The word is from the Greek mys, "muscle" and astheneia "weakness", and the Latin gravis, "serious".[15]
Signs and symptoms
[edit]The initial, main symptom in MG is painless weakness of specific muscles, not fatigue.[16] The muscle weakness becomes progressively worse (fatigue) during periods of physical activity and improves after periods of rest. Typically, the weakness and fatigue are worse toward the end of the day.[17] MG generally starts with ocular (eye) weakness; it might then progress to a more severe generalized form, characterized by weakness in the extremities or in muscles that govern basic life functions.[18]
Eyes
[edit]In about two-thirds of individuals, the initial symptom of MG is related to the muscles around the eye.[16] Eyelid drooping (ptosis may occur due to weakness of m. levator palpebrae superioris)[19] and double vision (diplopia,[16] due to weakness of the extraocular muscles).[17] Eye symptoms tend to get worse when watching television, reading, or driving, particularly in bright conditions.[16] Consequently, some affected individuals choose to wear sunglasses.[16] The term "ocular myasthenia gravis" describes a subtype of MG where muscle weakness is confined to the eyes, i.e. extraocular muscles, m. levator palpebrae superioris, and m. orbicularis oculi.[19] Typically, this subtype evolves into generalized MG, usually after a few years.[19]
Eating
[edit]The weakness of the muscles involved in swallowing may lead to swallowing difficulty (dysphagia). Typically, this means that some food may be left in the mouth after an attempt to swallow,[20] or food and liquids may regurgitate into the nose rather than go down the throat (velopharyngeal insufficiency).[17] Weakness of the muscles that move the jaw (muscles of mastication) may cause difficulty chewing. In individuals with MG, chewing tends to become more tiring when chewing tough, fibrous foods.[16] Difficulty in swallowing, chewing, and speaking is the first symptom in about one-sixth of individuals.[16]
Speaking
[edit]Weakness of the muscles involved in speaking may lead to dysarthria and hypophonia.[16] Speech may be slow and slurred,[21] or have a nasal quality.[17] In some cases, a singing hobby or profession must be abandoned.[20]
Head and neck
[edit]Due to weakness of the muscles of facial expression and muscles of mastication, facial weakness may manifest as the inability to hold the mouth closed[16] (the "hanging jaw sign") and as a snarling expression when attempting to smile.[17] With drooping eyelids, facial weakness may make the individual appear sleepy or sad.[16] Difficulty in holding the head upright may occur.[21]
Other
[edit]The muscles that control breathing and limb movements can also be affected; rarely do these present as the first symptoms of MG, but develop over months to years.[22] In a myasthenic crisis, a paralysis of the respiratory muscles occurs, necessitating assisted ventilation to sustain life.[23] Crises may be triggered by various biological stressors such as infection, fever, an adverse reaction to medication, or emotional stress.[23]
Cause
[edit]Medications that cause or worsen MG
[edit]Antibiotics: In the macrolide family of antibiotics, azithromycin, telithromycin (which is no longer available in the U.S. market), and erythromycin are reported to exacerbate MG. In the fluoroquinolone antibiotic family, ciprofloxacin, norfloxacin, ofloxacin, moxifloxacin, and moxifloxacin are reported to exacerbate MG.[24] And, In the aminoglycoside family of antibiotics, gentamicin, streptomycin, and neomycin are reported to exacerbate MG.[25] The aminoglycoside tobramycin has not been reported to exacerbate MG and may be used in patients that require aminoglycoside treatment.[24] Because of the rarity or absent reports on their exacerbation of MG, the following antibiotics are considered safe to use in MG patients: the cephalosporin class of drugs, sulfa drugs, the tetracycline group of drugs, clindamycin, polymyxin B, and nitrofurantoin.[24]
Immune checkpoint inhibitors: Immune checkpoint inhibitors promote certain types of autoimmune responses by blocking checkpoint pathways that inhibit these responses. They are used to treat cancers that promote their own growth and spread by stimulating checkpoint pathways. These checkpoint inhibitors include pembrolizumab, nivolumab, ipilimumab, avelumab, atezolizumab, and durvalumab. From a total 5,898 patients who received these drugs, 52 developed new onset MG and 11 had a flare of their preexisting MG. The symptoms of MG developed within 6 days to 16 weeks (median time 4 weeks). Their medicine-induced MG symptoms were often sever with 29 patients developing respiratory failure that required mechanical ventilation.[26] Other studies have reported that these checkpoint inhibitors cause respiratory failure in 45% and death in 25–40% of patients.[24][27] These medications, it is suggested, are best avoided in MG patients, particularly in patients who previously had a life-threatening reaction to them. If these medications must be used in MG patients, it is recommended that the patients be pre-treated with a glucocorticoid, plasmapheresis, or intravenous immunoglobulin to reduce the chances of their developing severe symptoms.[24]
Statins: Statins are drugs that lower blood cholesterol levels. In a review of 169 patients who were reported to develop MG or had worsened MG symptoms while taking a statin (i.e., simvastatin, atorvastatin, rosuvastatin, pravastatin, lovastatin, or fluvastatin), 138 had developed generalized MG, 13 had developed ocular MG, and 18 had worsening of their MG. Following discontinuance of the statin and treatment of their MG, 63 patients fully recovered, 27 patients were recovering, 19 patients had not yet recovered, 5 patients recovered but had ongoing symptoms, 1 patient had died, and there was no follow-up data for 54 patients. Among these cases, 56% were considered to be serious.[28] Non-statin cholesterol-lowering drugs, (e.g., niacin and the bile acid sequestrants drugs cholestyramine, colestipol, colesevelam, alirocumab, and evolocumab) have been used in patients without causing or worsening MG. It is advised that a statin be discontinued and thereafter all statins be avoided in the rare cases where the statin caused the development or worsening of MG.[24]
Ia antiarrhythmic agents: A type Ia antiarrhythmic agent (see Vaughan Williams classification), i.e., procainamide, which is used to treat cardiac arrhythmias, has caused respiratory failure in MG patients who, prior to being treated with it, did not have respiratory symptoms. Furthermore, this drug has caused MG-like symptoms in patients who have kidney failure but do not have MG. And, procainamide worsened muscle dysfunction in a rat model of human MG. These studies suggest that procainamide as well as other type Ia antiarrhythmic agents should be avoided or used with extreme caution in MG patients.[24]
Depolarizing neuromuscular blockers: Depolarizing neuromuscular blockers suppress the neurons' signaling at neuromuscular junctions thereby reducing the affected skeletal muscles contractibility. These blockers are used as muscle relaxants in patients undergoing surgery.[29] Succinylcholine is the only depolarizing neuromuscular blocker available in the U.S. market.[24] Succinylcholine's ability to induce or worsen MG is unclear. It has been suggested to cause life-threatening side effects such as rhabdomyolysis, myotonia, and hyperkalemia in patients with muscle disease although the role of succinylcholine in causing these side effects also remains unclear.[29] Until more evidence on these issues becomes available and since there are other neuromuscular blocking agents without these deleterious side effects, the use of succinylcholine in MG (and other neuromuscular disorders) should probably be avoided where feasible.[24][29]
Inhalation anesthetics: Inhalation anesthetics are general anesthetics that are delivered by inhalation generally for patients undergoing surgery. MG patients undergoing surgery with inhaled anesthetics (i.e., halothane, isoflurane, enflurane, and sevoflurane) may develop neuromuscular blockage and have an increased incidence of developing a life-threatening myasthenia crisis which must be treated by prolonged mechanical ventilation. In a study of 795 MG patients undergoing surgical removal of their thymus under general anesthesia, sugammadex, a neuromuscular-blocking drug (i.e., a drug that reverses neuromuscular blockade) significantly reduced the development of this crisis.[24][30] These studies suggest that inhalation anesthetics are best avoided in MG patients but if used close post-operation monitoring should be conducted for MG patients being anesthetized with these agents[24] and sugammadex should be considered for routine use in MG patients anesthetized with these agents who undergo thymectomy[31] or other types of surgery.[24]
Glucocorticoids: Glucocorticoids are anti-inflammatory agents that in initial studies were used at high dosages and found to worsen MG in 25-75% of cases.[32] However, further studies found that glucocorticoids do have favorable effects on MG when taken long-term. Two glucocorticoids, oral prednisone and prednisolone, are now the first line immunosuppressive treatment for MG. To avoid exacerbation of MG, it is recommended that the corticosteroids should be started at a low dose and gradually increased to the dose achieving maximal responses. To achieve a faster therapeutic responses in cases with severe MG symptoms, it has been recommended to start with high doses of oral or intravenous glucocorticoids after first treating patients with plasmapheresis or intravenous immunoglobulin therapy, each of which reduces the chance of having a severe reaction to the corticosteroids.[24][33][34]
Calcium channel blockers: Calcium channel blockers (e.g., felodipine, nifedipine, and verapamil) are drugs that lower blood pressure in patients with hypertension. Felodipine and nifedipine are reported to worsen MG and nifedipine and verapamil are reported to cause respiratory failure in patients with severe generalized MG. MG patients, especially those who are in remission or have well-controlled disease, generally can be treated with these blockers using their lowest effective doses and close monitoring for the worsening of MG symptoms.[24]
Penicillamine: Penicillamine is a chelation therapy drug used to treat various diseases (e.g., Wilson's disease). About 1-2% of individuals treated long term with penicillamine develop MG and/or develop low concentrations of antibodies to AChR.[35] Their MG is often mild and predominantly ocular MG, becomes evident usually 6–7 months (range one month to 8 years) after starting the drug, and goes into complete remission in 70% of the cases within 6–10 months after discontinuing the drug. It is recommended that penicillamine be discontinued and thereafter avoided in patients who develop MG symptoms when treated with it.[24]
Botulinum toxin A: Botulinum toxin A (sold under the brand name Botox, Jeuveau, and Xeomin) blocks transmission at neuromuscular junctions to paralyze the muscles into which it is injected. Local botulinum toxin A injections for cosmetic purposes have on occasion caused weaknesses in distant muscles, symptoms resembling ocular or generalized MG in individuals with subclinical MG, and exacerbations of previously controlled MG. Botulinum toxin A has also been used to treat spasmodic torticollis (i.e., involuntarily neck turning), blepharospasm (involuntary contraction of the eye lids), and other uncontrolled facial muscle spasms in MG patients without side effects or with only short-lived dysphagia or diplopia. Botulinum toxin A treatment, it is suggested, is best avoided in MG patients but may be offered with caution to patients with mild or stable MG using gradual increases in its dosages and close monitoring.[24]
Magnesium: Magnesium is a chemical element that blocks skeletal muscle contraction by inhibiting the release or acetylcholine at the neuromuscular junction and also by lowering the sensitivity of these muscles to acetylcholine.[24] Respiratory failure has occurred after systemic use of magnesium (mainly in the form of intravenous magnesium sulfate injections) for pre-eclampsia and after magnesium replacement during the course of a hospitalization in patients with underlying MG.[24][36] It is suggested that magnesium when given intravenously or when given orally at high doses should be used with extreme caution in MG patients.[24]
Local anesthetics: Local anesthetics cause absence of pain and all other sensations in a specific body part without loss of consciousness. There are two broad classes of these anesthetics: esters (i.e., lidocaine, bupivacaine, etidocaine, levobupivacaine, mepivacaine, prilocaine, and ropivacain) and amides (i.e., procaine, cocaine, tetracaine benzocaine, and chloroprocaine). Ester local anesthetics are metabolized by pseudocholinesterases which in MG patients taking anticholinesterase drugs may lead to excessive levels of these ester anesthetics. Amide local anesthetics are not metabolized by psuedocholineesterases. Based on these considerations, amide local anesthetics are strongly preferred over ester local anesthetics in patients with MG.[37][38]
Other Drugs: Rare cases of MG exacerbations have been reported in patients treated with: 1) penicillins, i.e., ampicillin and amoxicillin; 2) anti-cancer medications, i.e., lorlatinib, nilotinib, imatinib (these three drugs are tyrosine kinase inhibitors that may also cause MG), dabrafenib, and trametinib; 3) antipsychotic drugs, i.e., chlorpromazine, pimozide, thioridazine, clozapine, olanzapine, haloperidol, quetiapine, risperidone, and olanzapine; 4) IFN-α (may also cause MG); and 5) the chemical element, lithium. These agents can be used in MG patients because reports on their exacerbation (or induction) of MG are rare.[24]
Pathophysiology
[edit]MG is an autoimmune synaptopathy. The disorder occurs when the immune system malfunctions and generates antibodies that attack the body's tissues. The antibodies in MG attack a normal human protein, the nicotinic acetylcholine receptor, or a related protein called MuSK, a muscle-specific kinase.[39][40] Other, less frequent antibodies are found against LRP4, agrin, and titin proteins.[8][41]
Human leukocyte antigen haplotypes are associated with increased susceptibility to myasthenia gravis and other autoimmune disorders. Relatives of people with myasthenia gravis have a higher percentage of other immune disorders.[42][43]
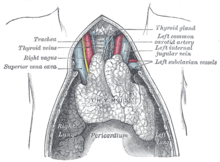
The thymus gland cells form part of the body's immune system. In those with myasthenia gravis, the thymus gland is large and abnormal. It sometimes contains clusters of immune cells that indicate lymphoid hyperplasia, and the thymus gland may give wrong instructions to immune cells.[44]
-
Neuromuscular junction: 1. Axon 2. Muscle cell membrane 3. Synaptic vesicle 4. Nicotinic acetylcholine receptor 5. Mitochondrion
-
A juvenile thymus shrinks with age.
In pregnancy
[edit]For women who are pregnant and already have MG, in a third of cases, they have been known to experience an exacerbation of their symptoms, and in those cases, it usually occurs in the first trimester of pregnancy.[45] Signs and symptoms in pregnant mothers tend to improve during the second and third trimesters. Complete remission can occur in some mothers.[46] Immunosuppressive therapy should be maintained throughout pregnancy, as this reduces the chance of neonatal muscle weakness, and controls the mother's myasthenia.[47]
About 10–20% of infants with mothers affected by the condition are born with transient neonatal myasthenia gravis (TNMG), which generally produces feeding and respiratory difficulties that develop about 12 hours to several days after birth.[45][47] A child with TNMG typically responds very well to acetylcholinesterase inhibitors, and the condition generally resolves over a period of three weeks, as the antibodies diminish, and generally does not result in any complications.[45] However, a small percentage of fetuses and newborns with TNMG, particularly those who have antibodies directed against the fetal form of the AChR (their disorder is a subtype of TNMG termed the "acetylcholine receptor inactivation syndrome") have a more severe form of TNMG which includes weakness in skeletal muscles regulating breathing, respiratory failure, and various deformities such as arthrogryposis multiplex congenita. In some of these cases, the mother remains asymptomatic.[47][48]
Diagnosis
[edit]MG can be difficult to diagnose, as the symptoms can be subtle and hard to distinguish from both normal variants and other neurological disorders.[20]
Three types of myasthenic symptoms in children can be distinguished:[49]
- Transient neonatal myasthenia gravis occurs in 10 to 15% of babies born to mothers afflicted with the disorder, and disappears after a few weeks.
- Congenital myasthenia, the rarest form, occurs when genes are present from both parents.
- Juvenile myasthenia gravis is most common in females.
Congenital myasthenias cause muscle weakness and fatigability similar to those of MG.[50] The signs of congenital myasthenia usually are present in the first years of childhood, although they may not be recognized until adulthood.[51]
Subgroup classification
[edit]| Class | Description |
|---|---|
| I | Any eye muscle weakness, possible ptosis, no other evidence of muscle weakness elsewhere |
| II | Eye muscle weakness of any severity, mild weakness of other muscles |
| IIa | Predominantly limb or axial muscles |
| IIb | Predominantly bulbar and/or respiratory muscles |
| III | Eye muscle weakness of any severity, moderate weakness of other muscles |
| IIIa | Predominantly limb or axial muscles |
| IIIb | Predominantly bulbar and/or respiratory muscles |
| IV | Eye muscle weakness of any severity, severe weakness of other muscles |
| IVa | Predominantly limb or axial muscles |
| IVb | Predominantly bulbar and/or respiratory muscles |
| V | Intubation needed to maintain airway |
When diagnosed with MG, patient can be stratified into distinct subgroups based on the clinical features and serological status, e.g. affected muscle group, age of onset, thymic abnormalities, and profile of serum autoantibodies.[53]
Based on the affected muscle group, patients can be sub-grouped into ocular MG or generalized MG. Ocular MG is characterized by exclusively ocular symptoms, droopy eyelids, or double vision. Generalized MG has muscle weakness with a variable combination of the bulbar, axial, or limb and respiratory muscles.[54]
Patients can also be sub-grouped by the age of onset: juvenile-onset MG (onset age ≤ 18 years of age), early-onset MG (EOMG; 19–50 years of age), late-onset MG (LOMG; onset > 50 years of age), and very late-onset (VLOMG; onset age ≥ 65 years of age).[55]
The subgroup of the autoantibody profile includes AChR seropositive, MuSK seropositive, LRP4 seropositive, and agrin seropositive.[56]
Physical examination
[edit]During a physical examination to check for MG, a doctor might ask the person to perform repetitive movements. For instance, the doctor may ask one to look at a fixed point for 30 seconds and to relax the muscles of the forehead, because a person with MG and ptosis of the eyes might be involuntarily using the forehead muscles to compensate for the weakness in the eyelids.[20] The clinical examiner might also try to elicit the "curtain sign" in a person by holding one of the person's eyes open, which in the case of MG will lead the other eye to close.[20]
Blood tests
[edit]If the diagnosis is suspected, serology can be performed:
- One test is for antibodies against the acetylcholine receptor;[20] the test has a reasonable sensitivity of 80–96%, but in ocular myasthenia, the sensitivity falls to 50%.
- A proportion of the people without antibodies against the acetylcholine receptor have antibodies against the MuSK protein.[57]
- In specific situations, testing is performed for Lambert-Eaton syndrome.[58]
Electrodiagnostics
[edit]

Muscle fibers of people with MG are easily fatigued, which the repetitive nerve stimulation test can help diagnose. In single-fiber electromyography, which is considered to be the most sensitive (although not the most specific) test for MG,[20] a thin needle electrode is inserted into different areas of a particular muscle to record the action potentials from several samplings of different individual muscle fibers. Two muscle fibers belonging to the same motor unit are identified, and the temporal variability in their firing patterns is measured. Frequency and proportion of particular abnormal action potential patterns, called "jitter" and "blocking", are diagnostic. Jitter refers to the abnormal variation in the time interval between action potentials of adjacent muscle fibers in the same motor unit. Blocking refers to the failure of nerve impulses to elicit action potentials in adjacent muscle fibers of the same motor unit.[59]
Ice test
[edit]Applying ice for 2–5 minutes to the muscles reportedly has a sensitivity and specificity of 76.9% and 98.3%, respectively, for the identification of MG. Acetylcholinesterase is thought to be inhibited at the lower temperature, which is the basis for this diagnostic test. This generally is performed on the eyelids when ptosis is present and is deemed positive if a ≥2-mm rise in the eyelid occurs after the ice is removed.[60]
Edrophonium test
[edit]This test requires the intravenous administration of edrophonium chloride or neostigmine, drugs that block the breakdown of acetylcholine by cholinesterase (acetylcholinesterase inhibitors).[61] This test is no longer typically performed, as its use can lead to life-threatening bradycardia (slow heart rate) which requires immediate emergency attention.[62] Production of edrophonium was discontinued in 2008.[23]
Imaging
[edit]A chest X-ray may identify widening of the mediastinum suggestive of thymoma, but computed tomography or magnetic resonance imaging (MRI) are more sensitive ways to identify thymomas and are generally done for this reason.[63] MRI of the cranium and orbits may also be performed to exclude compressive and inflammatory lesions of the cranial nerves and ocular muscles.[64]
Pulmonary function test
[edit]The forced vital capacity may be monitored at intervals to detect increasing muscular weakness. Acutely, negative inspiratory force may be used to determine adequacy of ventilation; it is performed on those individuals with MG.[65][66]
Differential diagnoses
[edit]The muscle weakness that worsens with activity (abnormal muscle fatigue) in myasthenia gravis[67] is a symptom shared by other neuromuscular diseases. Most of the metabolic myopathies, such as McArdle disease (GSD-V), have abnormal muscle fatigue rather than fixed muscle weakness.[68][69] Also, like myasthenia gravis,[67] exercise intolerance in McArdle disease improves with regular physical activity (performed safely using activity adaptations such as getting into second wind, the "30 for 80 rule," and "six second rule").[70][71] A small minority of patients with McArdle disease also have the comorbidity of ptosis (drooping upper eyelid).[72] Late-onset GSD-II (Pompe disease) and GSD-XV also have muscle weakness or fatigue with comorbidities of ptosis and ophthalmoplegia; as do many of the mitochondrial myopathies.[73]
Other diseases that involve abnormal muscle fatigue (which may be described as exercise-induced muscle weakness, reversible muscle weakness, or muscle weakness that improves with rest) include: endocrine myopathies (such as Hoffman syndrome), Tubular aggregate myopathy (TAM), ischemia (such as intermittent claudication, popliteal artery entrapment syndrome, and chronic venous insufficiency), and poor diet or malabsorption diseases that lead to vitamin D deficiency (osteomalic myopathy). Although limb-girdle muscular dystrophies (LGMDs) involve fixed muscle weakness, LGMDR8 also involves muscle fatigue;[74] as do some limb-girdle muscular dystrophy-dystroglycanopathies such as MDDGC3 (a.k.a. LGMDR15 and LGMD2O).[73][75] Myofibrillar myopathy 10,[76] dimethylglycine dehydrogenase deficiency,[77] erythrocyte lactate transporter defect,[78] and myopathy with myalgia, increased serum creatine kinase, with or without episodic rhabdomyolysis (MMCKR)[79] also include muscle fatigue.
X-linked episodic muscle weakness (EMWX) includes general muscle weakness, ptosis, and fluctuations in strength. In some individuals, fatiguability was demonstrable, the phenotype having features comparable to congenital myasthenic syndromes and channelopathies.[80]
Signs and symptoms of myasthenia presenting from infancy or childhood may be one of the congenital myasthenic syndromes, which can be inherited in either an autosomal dominant or recessive manner. There are currently over two dozen types of congenital myasthenic syndromes.[81]
Limb–girdle myasthenia gravis is a distinct condition from myasthenia gravis. It is an adult-onset, autoimmune condition affecting the neuromuscular junction. However, it lacks eye abnormalities and is associated with autoimmune conditions such as systemic lupus erythematosus, Hashimoto's thyroiditis, and thymoma.[82]
Lambert–Eaton myasthenic syndrome (LEMS) is an autoimmune condition that attacks the neuromuscular junction, either as a paraneoplastic syndrome (typically older patients) or associated with a non-cancerous primary autoimmune condition (typically younger patients). It usually involves lower limb weakness and exercise-induced fatiguability, although the upper limbs and eyes may also be involved. Lambert's sign is the unusual improvement of grip strength that follows after squeezing the hand at maximum intensity for 2–3 seconds.[83]
Management
[edit]Treatment is by medication and/or surgery. Medication consists mainly of acetylcholinesterase inhibitors to directly improve muscle function and immunosuppressant drugs to reduce the autoimmune process.[5][84] Thymectomy is a surgical method to treat MG.[85]
Medication
[edit]

About 10% of people with generalized MG are considered treatment-refractory.[86] Autologous hematopoietic stem cell transplantation (HSCT) is sometimes used in severe, treatment-refractory MG. Available data provide preliminary evidence that HSCT can be an effective therapeutic option in carefully selected cases.[87]
Efgartigimod alfa (Vyvgart) was approved for medical use in the United States in December 2021.[88][89][90]
Efgartigimod alfa/hyaluronidase (Vyvgart Hytrulo) was approved for medical use in the United States in June 2023.[91][92]
Rozanolixizumab (Rystiggo) was approved for medical use in the United States in June 2023.[93][94]
Acetylcholinesterase inhibitors
[edit]Acetylcholinesterase inhibitors can provide symptomatic benefit and may not fully remove a person's weakness from MG.[95] While they might not fully remove all symptoms of MG, they still may allow a person the ability to perform normal daily activities.[95] Usually, acetylcholinesterase inhibitors are started at a low dose and increased until the desired result is achieved. If taken 30 minutes before a meal, symptoms will be mild during eating, which is helpful for those who have difficulty swallowing due to their illness. Another medication used for MG, atropine, can reduce the muscarinic side effects of acetylcholinesterase inhibitors.[96] Pyridostigmine is a relatively long-acting drug (when compared to other cholinergic agonists), with a half-life around four hours with relatively few side effects.[97] Generally, it is discontinued in those who are being mechanically ventilated, as it is known to increase the amount of salivary secretions.[97] A few high-quality studies have directly compared cholinesterase inhibitors with other treatments (or placebo); their practical benefit may be so significant that conducting studies in which they would be withheld from some people would be difficult.[84]
Immune suppressants
[edit]The steroid prednisone might also be used to achieve a better result, but it can lead to the worsening of symptoms and takes weeks to achieve its maximal effectiveness.[97] Research suggests that up to 15% of patients do not positively respond to immune suppressants.[98][99][5] Due to the myriad symptoms that steroid treatments can cause, it is not the preferred method of treatment.[97] Other immune suppressing medications may also be used including rituximab[100] or azathioprine.[1]
Plasmapheresis and IVIG
[edit]If the myasthenia is serious (myasthenic crisis), plasmapheresis can be used to remove the putative antibodies from the circulation. Also, intravenous immunoglobulins (IVIGs) can be used to bind the circulating antibodies. Both of these treatments have relatively short-lived benefits, typically measured in weeks, and often are associated with high costs, which make them prohibitive; they are generally reserved for when MG requires hospitalization.[97][101]
Surgery
[edit]As thymomas are seen in 10% of all people with the MG, they are often given a chest X-ray and CT scan to evaluate their need for surgical removal of their thymus glands and any cancerous tissue that may be present.[23][62] Even if surgery is performed to remove a thymoma, it generally does not lead to the remission of MG.[97] Surgery in the case of MG involves the removal of the thymus, although in 2013, no clear benefit was indicated except in the presence of a thymoma.[102] A 2016 randomized, controlled trial, however, found some benefits.[103]
Physical measures
[edit]People with MG should be educated regarding the fluctuating nature of their symptoms, including weakness and exercise-induced fatigue. Exercise participation should be encouraged with frequent rest.[18] In people with generalized MG, some evidence indicates a partial home program including training in diaphragmatic breathing, pursed-lip breathing, and interval-based muscle therapy may improve respiratory muscle strength, chest wall mobility, respiratory pattern, and respiratory endurance.[104]
Medical imaging
[edit]In people with myasthenia gravis, older forms of iodinated contrast used for medical imaging have caused an increased risk of exacerbation of the disease, but modern forms have no immediate increased risk.[105]
Prognosis
[edit]The prognosis of people with MG is generally good, as is quality of life, when given very good treatment.[106] Monitoring of a person with MG is very important, as at least 20% of people diagnosed with it will experience a myasthenic crisis within two years of their diagnosis, requiring rapid medical intervention.[97] Generally, the most disabling period of MG might be years after the initial diagnosis.[95] Assistive devices may be needed to assist with mobility.[1] In the early 1900s, 70% of detected cases died from lung problems; now, that number is estimated to be around 3–5%, an improvement attributed to increased awareness and medications to manage symptoms.[97]
Epidemiology
[edit]MG occurs in all ethnic groups and both sexes. It most commonly affects women under 40 and people from 50 to 70 years old of either sex, but it has been known to occur at any age. Younger people rarely have thymoma. Prevalence in the United States is estimated at between 0.5 and 20.4 cases per 100,000, with an estimated 60,000 Americans affected.[23][107] In the United Kingdom, an estimated 15 cases of MG occur per 100,000 people.[62] The mortality rate of MG is around 5-9%.[108]
History
[edit]The first to write about MG were Thomas Willis, Samuel Wilks, Erb, and Goldflam.[19] The term "myasthenia gravis pseudo-paralytica" was proposed in 1895 by Jolly, a German physician.[19] Mary Walker treated a person with MG with physostigmine in 1934.[19] Simpson and Nastuck detailed the autoimmune nature of the condition.[19] In 1973, Patrick and Lindstrom used rabbits to show that immunization with purified muscle-like acetylcholine receptors caused the development of MG-like symptoms.[19]
Research
[edit]Immunomodulating substances, such as drugs that prevent acetylcholine receptor modulation by the immune system, are currently being researched.[109] Some research recently has been on anti-c5 inhibitors for treatment research as they are safe and used in the treatment of other diseases.[14] Ephedrine seems to benefit some people more than other medications, but it has not been properly studied as of 2014.[10][110] In the laboratory, MG is mostly studied in model organisms, such as rodents. In addition, in 2015, scientists developed an in vitro functional, all-human, neuromuscular junction assay from human embryonic stem cells and somatic-muscle stem cells. After the addition of pathogenic antibodies against the acetylcholine receptor and activation of the complement system, the neuromuscular co-culture shows symptoms such as weaker muscle contractions.[111] Recent years, scientists have been working on finding the reliable biomarkers for MG to monitor the disease development and assess the severity.
References
[edit]- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z "Myasthenia Gravis Fact Sheet". National Institute of Neurological Disorders and Stroke. Archived from the original on 16 September 2021. Retrieved 22 September 2021.
- ^ Kahan S (2005). In a Page: Neurology. Lippincott Williams & Wilkins. p. 118. ISBN 978-1-4051-0432-6. Archived from the original on 8 September 2017.
- ^ a b Kaminski HJ (2009). Myasthenia Gravis and Related Disorders (2 ed.). Springer Science & Business Media. p. 72. ISBN 978-1-59745-156-7. Archived from the original on 8 September 2017.
- ^ a b Adams JG (2012). Emergency Medicine: Clinical Essentials (2 ed.). Elsevier Health Sciences. p. 844. ISBN 978-1-4557-3394-1. Archived from the original on 8 September 2017.
- ^ a b c d Salari N, Fatahi B, Bartina Y, Kazeminia M, Fatahian R, Mohammadi P, et al. (December 2021). "Global prevalence of myasthenia gravis and the effectiveness of common drugs in its treatment: a systematic review and meta-analysis". Journal of Translational Medicine. 19 (1): 516. doi:10.1186/s12967-021-03185-7. PMC 8686543. PMID 34930325.
- ^ Young C, McGill SC (April 2021). Rituximab for the Treatment of Myasthenia Gravis: A 2021 Update [Internet] (Report). Ottawa (ON): Canadian Agency for Drugs and Technologies in Health. PMID 34255447. Archived from the original on 7 July 2022. Retrieved 27 January 2022.
- ^ Dabi A, Solieman N, Kurukumbi M, Kalyanam J (2012). "Myasthenia Gravis: A Review". Autoimmune Diseases. 2012: 1–10. doi:10.1155/2012/874680. PMC 3501798. PMID 23193443.
- ^ a b Phillips WD, Vincent A (1 January 2016). "Pathogenesis of myasthenia gravis: update on disease types, models, and mechanisms". F1000Research. 5: 1513. doi:10.12688/f1000research.8206.1. PMC 4926737. PMID 27408701.
- ^ Kandel E, Schwartz J, Jessel T, Siegelbaum S, Hudspeth A (2012). Principles of Neural Science (5 ed.). pp. 318–319.
- ^ a b Vrinten C, van der Zwaag AM, Weinreich SS, Scholten RJ, Verschuuren JJ (December 2014). "Ephedrine for myasthenia gravis, neonatal myasthenia and the congenital myasthenic syndromes". The Cochrane Database of Systematic Reviews. 2014 (12): CD010028. doi:10.1002/14651858.CD010028.pub2. PMC 7387729. PMID 25515947.
- ^ Lindroos JL, Bjørk MH, Gilhus NE (February 2024). "Transient Neonatal Myasthenia Gravis as a Common Complication of a Rare Disease: A Systematic Review". Journal of Clinical Medicine. 13 (4): 1136. doi:10.3390/jcm13041136. PMC 10889526. PMID 38398450.
- ^ Godoy DA, Mello LJ, Masotti L, Di Napoli M (September 2013). "The myasthenic patient in crisis: an update of the management in Neurointensive Care Unit". Arquivos de Neuro-Psiquiatria. 71 (9A): 627–39. doi:10.1590/0004-282X20130108. PMID 24141444.
- ^ a b McGrogan A, Sneddon S, de Vries CS (2010). "The incidence of myasthenia gravis: a systematic literature review". Neuroepidemiology. 34 (3): 171–183. doi:10.1159/000279334. PMID 20130418. S2CID 34447321.
- ^ a b Conti-Fine BM, Milani M, Kaminski HJ (November 2006). "Myasthenia gravis: past, present, and future". The Journal of Clinical Investigation. 116 (11): 2843–2854. doi:10.1172/JCI29894. PMC 1626141. PMID 17080188.
- ^ Ehrlich A, Schroeder CL (2014). Introduction to Medical Terminology. Cengage Learning. p. 87. ISBN 978-1-133-95174-2. Archived from the original on 8 September 2017.
- ^ a b c d e f g h i j Engel AG (2012). Myasthenia Gravis and Myasthenic Disorders (2nd ed.). Oxford University Press, US. pp. 109–110. ISBN 978-0-19-973867-0. Archived from the original on 8 September 2017.
- ^ a b c d e Scully C (2014). Scully's Medical Problems in Dentistry. Elsevier Health Sciences UK. ISBN 978-0-7020-5963-6. Archived from the original on 8 September 2017.
- ^ a b Myasthenia Gravis at eMedicine
- ^ a b c d e f g h Nair AG, Patil-Chhablani P, Venkatramani DV, Gandhi RA (October 2014). "Ocular myasthenia gravis: a review". Indian Journal of Ophthalmology. 62 (10): 985–991. doi:10.4103/0301-4738.145987. PMC 4278125. PMID 25449931.
- ^ a b c d e f g Scherer K, Bedlack RS, Simel DL (April 2005). "Does this patient have myasthenia gravis?". JAMA. 293 (15): 1906–1914. doi:10.1001/jama.293.15.1906. PMID 15840866.
- ^ a b Rajendran A; Sundaram S (2014). Shafer's Textbook of Oral Pathology (7th ed.). Elsevier Health Sciences APAC. p. 867. ISBN 978-81-312-3800-4. Archived from the original on 2 April 2017.
- ^ MedlinePlus Encyclopedia: Myasthenia gravis
- ^ a b c d e Marx JA (2014). Rosen's emergency medicine: concepts and clinical practice (8th ed.). Philadelphia: Elsevier/Saunders. pp. 1441–1444. ISBN 978-1-4557-0605-1.
- ^ a b c d e f g h i j k l m n o p q r s t Sheikh S, Alvi U, Soliven B, Rezania K (April 2021). "Drugs That Induce or Cause Deterioration of Myasthenia Gravis: An Update". Journal of Clinical Medicine. 10 (7): 1537. doi:10.3390/jcm10071537. PMC 8038781. PMID 33917535.
- ^ Hall DR, McGibbon DH, Evans CC, Meadows GA (December 1972). "Gentamicin, tubocurarine, lignocaine and neuromuscular blockade. A case report". British Journal of Anaesthesia. 44 (12): 1329–32. doi:10.1093/bja/44.12.1329. PMID 4568132.
- ^ Safa H, Johnson DH, Trinh VA, Rodgers TE, Lin H, Suarez-Almazor ME, Fa'ak F, Saberian C, Yee C, Davies MA, Tummala S, Woodman K, Abdel-Wahab N, Diab A (November 2019). "Immune checkpoint inhibitor related myasthenia gravis: single center experience and systematic review of the literature". Journal for Immunotherapy of Cancer. 7 (1): 319. doi:10.1186/s40425-019-0774-y. PMC 6868691. PMID 31753014.
- ^ Puwanant A, Isfort M, Lacomis D, Živković SA (February 2019). "Clinical spectrum of neuromuscular complications after immune checkpoint inhibition". Neuromuscular Disorders. 29 (2): 127–133. doi:10.1016/j.nmd.2018.11.012. PMID 30638612.
- ^ Gras-Champel V, Batteux B, Masmoudi K, Liabeuf S (October 2019). "Statin-induced myasthenia: A disproportionality analysis of the WHO's VigiBase pharmacovigilance database". Muscle & Nerve. 60 (4): 382–386. doi:10.1002/mus.26637. PMID 31298743.
- ^ a b c van den Bersselaar LR, Gubbels M, Riazi S, Heytens L, Jungbluth H, Voermans NC, Snoeck MM (June 2022). "Mapping the current evidence on the anesthetic management of adult patients with neuromuscular disorders-a scoping review". Canadian Journal of Anaesthesia = Journal Canadien d'Anesthesie. 69 (6): 756–773. doi:10.1007/s12630-022-02230-3. PMC 9132812. PMID 35322378.
- ^ Mouri H, Jo T, Matsui H, Fushimi K, Yasunaga H (February 2020). "Effect of Sugammadex on Postoperative Myasthenic Crisis in Myasthenia Gravis Patients: Propensity Score Analysis of a Japanese Nationwide Database". Anesthesia and Analgesia. 130 (2): 367–373. doi:10.1213/ANE.0000000000004239. PMID 31124838.
- ^ Cata JP, Lasala JD, Williams W, Mena GE (September 2019). "Myasthenia Gravis and Thymoma Surgery: A Clinical Update for the Cardiothoracic Anesthesiologist". Journal of Cardiothoracic and Vascular Anesthesia. 33 (9): 2537–2545. doi:10.1053/j.jvca.2018.07.036. PMID 30219643.
- ^ Hoffmann S, Kohler S, Ziegler A, Meisel A (October 2014). "Glucocorticoids in myasthenia gravis - if, when, how, and how much?". Acta Neurologica Scandinavica. 130 (4): 211–21. doi:10.1111/ane.12261. PMID 25069701.
- ^ Dalakas MC, Meisel A (April 2022). "Immunomodulatory effects and clinical benefits of intravenous immunoglobulin in myasthenia gravis". Expert Review of Neurotherapeutics. 22 (4): 313–318. doi:10.1080/14737175.2022.2057223. PMID 35350948.
- ^ Ghimire A, Kunwar B, Aryal B, Gaire A, Bist A, Shah B, Mainali A, Ghimire B, Gajurel BP (March 2024). "Assessing the comparative efficacy of plasmapheresis and Intravenous immunoglobulin in myasthenia gravis treatment: A systematic review and meta-analysis". Journal of Clinical Neuroscience. 121: 1–10. doi:10.1016/j.jocn.2024.01.025. PMID 38306763.
- ^ Vincent A, Palace J, Hilton-Jones D (June 2001). "Myasthenia gravis". Lancet. 357 (9274): 2122–8. doi:10.1016/S0140-6736(00)05186-2. PMID 11445126.
- ^ Petrucelli N, Barra ME, Koehl JL (January 2024). "Evaluation of Medication Exposure on Exacerbation of Disease in Patients With Myasthenia Gravis". The Neurohospitalist. 14 (1): 52–57. doi:10.1177/19418744231206256. PMC 10790617. PMID 38235027.
- ^ Muckler VC, O'Brien JM, Matson SE, Rice AN (February 2019). "Perianesthetic Implications and Considerations for Myasthenia Gravis". Journal of Perianesthesia Nursing. 34 (1): 4–15. doi:10.1016/j.jopan.2018.03.009. PMID 29980408.
- ^ Prabhu SS, Khan SA, Doudnikoff AL, Reebye UN (February 2019). "Anesthetic considerations for a patient with myasthenia gravis undergoing deep sedation in an outpatient oral surgery setting". Journal of Dental Anesthesia and Pain Medicine. 19 (1): 67–72. doi:10.17245/jdapm.2019.19.1.67. PMC 6405345. PMID 30859135.
- ^ Valenzuela DM, Stitt TN, DiStefano PS, Rojas E, Mattsson K, Compton DL, Nunez L, Park JS, Stark JL, Gies DR, Thomas S, LeBeau MM, Fernald AA, Copeland NG, Jenkins NA, Burden SJ, Glass DJ, Yancopoulos GD (September 1995). "Receptor tyrosine kinase specific for the skeletal muscle lineage: expression in embryonic muscle, at the neuromuscular junction, and after injury". Neuron. 15 (3): 573–584. doi:10.1016/0896-6273(95)90146-9. PMID 7546737. S2CID 17575761.
- ^ "Myasthenia gravis". Genetics Home Reference. Archived from the original on 11 July 2015. Retrieved 10 July 2015.
- ^ Sinmaz N, Nguyen T, Tea F, Dale RC, Brilot F (August 2016). "Mapping autoantigen epitopes: molecular insights into autoantibody-associated disorders of the nervous system". Journal of Neuroinflammation. 13 (1): 219. doi:10.1186/s12974-016-0678-4. PMC 5006540. PMID 27577085.
- ^ Sathasivam S (January 2014). "Diagnosis and management of myasthenia gravis". Progress in Neurology and Psychiatry. 18 (1): 6–14. doi:10.1002/pnp.315. S2CID 115659064.
- ^ "Myasthenia Gravis". PubMed Health. Bethesda, MD: U.S. National Library of Medicine. Archived from the original on 18 October 2016. Retrieved 9 July 2015.
- ^ "Myasthenia Gravis Fact Sheet". www.ninds.nih.gov. National Institute of Neurological Disorders and Stroke (NINDS). Archived from the original on 11 July 2015. Retrieved 10 July 2015.
- ^ a b c Varner M (June 2013). "Myasthenia gravis and pregnancy". Clinical Obstetrics and Gynecology. 56 (2): 372–81. doi:10.1097/GRF.0b013e31828e92c0. PMID 23563874.
- ^ Téllez-Zenteno JF, Hernández-Ronquillo L, Salinas V, Estanol B, da Silva O (November 2004). "Myasthenia gravis and pregnancy: clinical implications and neonatal outcome". BMC Musculoskeletal Disorders. 5 (1): 42. doi:10.1186/1471-2474-5-42. PMC 534111. PMID 15546494.
- ^ a b c Warrell DA, Cox TM, et al. (2003). Oxford Textbook of Medicine. Vol. 3 (Fourth ed.). Oxford. p. 1170. ISBN 978-0-19-852787-9.
- ^ Allen NM, O'Rahelly M, Eymard B, Chouchane M, Hahn A, Kearns G, Kim DS, Byun SY, Nguyen CE, Schara-Schmidt U, Kölbel H, Marina AD, Schneider-Gold C, Roefke K, Thieme A, Van den Bergh P, Avalos G, Álvarez-Velasco R, Natera-de Benito D, Cheng MH, Chan WK, Wan HS, Thomas MA, Borch L, Lauzon J, Kornblum C, Reimann J, Mueller A, Kuntzer T, Norwood F, Ramdas S, Jacobson LW, Jie X, Fernandez-Garcia MA, Wraige E, Lim M, Lin JP, Claeys KG, Aktas S, Oskoui M, Hacohen Y, Masud A, Leite MI, Palace J, De Vivo D, Vincent A, Jungbluth H (October 2023). "The emerging spectrum of fetal acetylcholine receptor antibody-related disorders (FARAD)". Brain: A Journal of Neurology. 146 (10): 4233–4246. doi:10.1093/brain/awad153. PMC 10545502. PMID 37186601.
- ^ Rudd K, Kocisko D (2013). Pediatric Nursing: The Critical Components of Nursing Care. F.A. Davis. ISBN 978-0-8036-4053-5. Archived from the original on 3 June 2016.
- ^ Engel AG, Shen XM, Selcen D, Sine SM (April 2015). "Congenital myasthenic syndromes: pathogenesis, diagnosis, and treatment". The Lancet. Neurology. 14 (4): 420–434. doi:10.1016/S1474-4422(14)70201-7. PMC 4520251. PMID 25792100.
- ^ "Congenital Myasthenia Information Page: National Institute of Neurological Disorders and Stroke (NINDS)". www.ninds.nih.gov. Archived from the original on 12 July 2015. Retrieved 11 July 2015.
- ^ Wolfe GI, Barohn RJ (2009). "Myasthenia Gravis: Classification and Outcome Measurements". Myasthenia Gravis and Related Disorders. pp. 293–302. doi:10.1007/978-1-59745-156-7_18. ISBN 978-1-58829-852-2.
- ^ Meriggioli, Matthew N; Sanders, Donald B (May 2009). "Autoimmune myasthenia gravis: emerging clinical and biological heterogeneity". The Lancet Neurology. 8 (5): 475–490. doi:10.1016/S1474-4422(09)70063-8. PMC 2730933. PMID 19375665.
- ^ Gilhus, Nils Erik; Verschuuren, Jan J (October 2015). "Myasthenia gravis: subgroup classification and therapeutic strategies". The Lancet Neurology. 14 (10): 1023–1036. doi:10.1016/s1474-4422(15)00145-3. ISSN 1474-4422. PMID 26376969.
- ^ Punga, Anna Rostedt; Maddison, Paul; Heckmann, Jeannine M; Guptill, Jeffrey T; Evoli, Amelia (February 2022). "Epidemiology, diagnostics, and biomarkers of autoimmune neuromuscular junction disorders". The Lancet Neurology. 21 (2): 176–188. doi:10.1016/S1474-4422(21)00297-0. PMID 35065040.
- ^ Koneczny, Inga; Herbst, Ruth (2 July 2019). "Myasthenia Gravis: Pathogenic Effects of Autoantibodies on Neuromuscular Architecture". Cells. 8 (7): 671. doi:10.3390/cells8070671. ISSN 2073-4409. PMC 6678492. PMID 31269763.
- ^ Leite MI, Jacob S, Viegas S, Cossins J, Clover L, Morgan BP, et al. (July 2008). "IgG1 antibodies to acetylcholine receptors in 'seronegative' myasthenia gravis". Brain. 131 (Pt 7): 1940–52. doi:10.1093/brain/awn092. PMC 2442426. PMID 18515870.
- ^ MedlinePlus Encyclopedia: Lambert-Eaton syndrome
- ^ Selvan VA (January 2011). "Single-fiber EMG: A review". Annals of Indian Academy of Neurology. 14 (1): 64–67. doi:10.4103/0972-2327.78058. PMC 3108086. PMID 21654930.
- ^ Kearsey C, Fernando P, D'Costa D, Ferdinand P (June 2010). "The use of the ice pack test in myasthenia gravis". JRSM Short Reports. 1 (1): 14. doi:10.1258/shorts.2009.090037. PMC 2984327. PMID 21103106.
- ^ MedlinePlus Encyclopedia: Tensilon test
- ^ a b c Spillane J, Higham E, Kullmann DM (December 2012). "Myasthenia gravis". BMJ. 345 (dec21 3): e8497. doi:10.1136/bmj.e8497. PMID 23261848. S2CID 13911967.
- ^ de Kraker M, Kluin J, Renken N, Maat AP, Bogers AJ (June 2005). "CT and myasthenia gravis: correlation between mediastinal imaging and histopathological findings". Interactive Cardiovascular and Thoracic Surgery. 4 (3): 267–271. doi:10.1510/icvts.2004.097246. PMID 17670406.
- ^ Allan H. Ropper, Robert H. Brown Adams and Victor's Principles of Neurology McGraw-Hill Professional; 8 edition (2005)
- ^ MedlinePlus Encyclopedia: Pulmonary function tests
- ^ Emergent Management of Myasthenia Gravis at eMedicine
- ^ a b Gilhus, Nils Erik (1 March 2021). "Physical training and exercise in myasthenia gravis". Neuromuscular Disorders. 31 (3): 169–173. doi:10.1016/j.nmd.2020.12.004. hdl:11250/2767222. ISSN 0960-8966. PMID 33461846. S2CID 229372884.
- ^ Darras, B. T.; Friedman, N. R. (February 2000). "Metabolic myopathies: a clinical approach; part I". Pediatric Neurology. 22 (2): 87–97. doi:10.1016/s0887-8994(99)00133-2. ISSN 0887-8994. PMID 10738913. Archived from the original on 24 May 2023. Retrieved 24 November 2023.
- ^ Tobon, Alejandro (December 2013). "Metabolic myopathies". Continuum (Minneapolis, Minn.). 19 (6 Muscle Disease): 1571–1597. doi:10.1212/01.CON.0000440660.41675.06. ISSN 1538-6899. PMC 10563931. PMID 24305448.
- ^ Wakelin, A. (2017). Living with McArdle Disease (PDF). IamGSD. Archived (PDF) from the original on 5 March 2023. Retrieved 24 November 2023.
- ^ Reason, S. L.; Voermans, N.; Lucia, A.; Vissing, J.; Quinlivan, R.; Bhai, S.; Wakelin, A. (July 2023). "Development of Continuum of Care for McArdle disease: A practical tool for clinicians and patients". Neuromuscular Disorders. 33 (7): 575–579. doi:10.1016/j.nmd.2023.05.006. ISSN 1873-2364. PMID 37354872. S2CID 259141690.
- ^ Scalco, Renata S.; Lucia, Alejandro; Santalla, Alfredo; Martinuzzi, Andrea; Vavla, Marinela; Reni, Gianluigi; Toscano, Antonio; Musumeci, Olimpia; Voermans, Nicol C.; Kouwenberg, Carlyn V.; Laforêt, Pascal; San-Millán, Beatriz; Vieitez, Irene; Siciliano, Gabriele; Kühnle, Enrico (24 November 2020). "Data from the European registry for patients with McArdle disease and other muscle glycogenoses (EUROMAC)". Orphanet Journal of Rare Diseases. 15 (1): 330. doi:10.1186/s13023-020-01562-x. ISSN 1750-1172. PMC 7687836. PMID 33234167.
- ^ a b Urtizberea, Jon Andoni; Severa, Gianmarco; Malfatti, Edoardo (May 2023). "Metabolic Myopathies in the Era of Next-Generation Sequencing". Genes. 14 (5): 954. doi:10.3390/genes14050954. ISSN 2073-4425. PMC 10217901. PMID 37239314.
- ^ "MUSCULAR DYSTROPHY, LIMB-GIRDLE, AUTOSOMAL RECESSIVE 8; LGMDR8". www.omim.org. Archived from the original on 31 May 2024. Retrieved 24 November 2023.
- ^ "MUSCULAR DYSTROPHY-DYSTROGLYCANOPATHY (LIMB-GIRDLE), TYPE C, 3; MDDGC3". www.omim.org. Archived from the original on 9 June 2023. Retrieved 24 November 2023.
- ^ "MYOFIBRILLAR MYOPATHY 10; MFM10". www.omim.org. Archived from the original on 21 April 2024. Retrieved 24 November 2023.
- ^ "DIMETHYLGLYCINE DEHYDROGENASE DEFICIENCY; DMGDHD". www.omim.org. Archived from the original on 14 October 2022. Retrieved 24 November 2023.
- ^ "ERYTHROCYTE LACTATE TRANSPORTER DEFECT". www.omim.org. Archived from the original on 13 May 2024. Retrieved 24 November 2023.
- ^ "MYOPATHY WITH MYALGIA, INCREASED SERUM CREATINE KINASE, AND WITH OR WITHOUT EPISODIC RHABDOMYOLYSIS; MMCKR". www.omim.org. Archived from the original on 3 June 2024. Retrieved 24 November 2023.
- ^ "EPISODIC MUSCLE WEAKNESS, X-LINKED; EMWX". www.omim.org. Archived from the original on 3 July 2024. Retrieved 24 November 2023.
- ^ "Phenotypic Series - PS601462, PS610542 - Congenital myasthenic syndromes - OMIM". www.omim.org. Archived from the original on 3 July 2024. Retrieved 24 November 2023.
- ^ "159400 - MYASTHENIA, LIMB-GIRDLE, AUTOIMMUNE - OMIM". www.omim.org. Archived from the original on 2 June 2023. Retrieved 29 February 2024.
- ^ Pascuzzi, Robert M.; Bodkin, Cynthia L. (2022). "Myasthenia Gravis and Lambert-Eaton Myasthenic Syndrome: New Developments in Diagnosis and Treatment". Neuropsychiatric Disease and Treatment. 18: 3001–3022. doi:10.2147/NDT.S296714. ISSN 1176-6328. PMC 9792103. PMID 36578903.
- ^ a b Mehndiratta MM, Pandey S, Kuntzer T (October 2014). "Acetylcholinesterase inhibitor treatment for myasthenia gravis". The Cochrane Database of Systematic Reviews. 2014 (10): CD006986. doi:10.1002/14651858.CD006986.pub3. PMC 7390275. PMID 25310725.
- ^ Gronseth GS, Barohn RJ (July 2000). "Practice parameter: thymectomy for autoimmune myasthenia gravis (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology". Neurology. 55 (1): 7–15. doi:10.1212/wnl.55.1.7. PMID 10891896.
- ^ Suh J, Goldstein JM, Nowak RJ (June 2013). "Clinical characteristics of refractory myasthenia gravis patients". The Yale Journal of Biology and Medicine. 86 (2): 255–60. PMC 3670444. PMID 23766745.
- ^ Burman J, Tolf A, Hägglund H, Askmark H (February 2018). "Autologous haematopoietic stem cell transplantation for neurological diseases". Journal of Neurology, Neurosurgery, and Psychiatry. 89 (2): 147–155. doi:10.1136/jnnp-2017-316271. PMC 5800332. PMID 28866625.
- ^
 This article incorporates text from this source, which is in the public domain: "FDA Approves New Treatment for Myasthenia Gravis". U.S. Food and Drug Administration (FDA) (Press release). 17 December 2021. Archived from the original on 20 December 2021. Retrieved 21 December 2021.
This article incorporates text from this source, which is in the public domain: "FDA Approves New Treatment for Myasthenia Gravis". U.S. Food and Drug Administration (FDA) (Press release). 17 December 2021. Archived from the original on 20 December 2021. Retrieved 21 December 2021.
- ^ "Argenx Announces U.S. Food and Drug Administration (FDA) Approval of Vyvgart (efgartigimod alfa-fcab) in Generalized Myasthenia Gravis". Argenx (Press release). 17 December 2021. Archived from the original on 20 December 2021. Retrieved 21 December 2021.
- ^ "argenx Announces U.S. Food and Drug Administration (FDA) Approval of Vyvgart (efgartigimod alfa-fcab) in Generalized Myasthenia Gravis" (Press release). Argenx. 17 December 2021. Archived from the original on 19 December 2021. Retrieved 21 December 2021 – via Business Wire.
- ^ "Halozyme Announces argenx Receives FDA Approval for Vyvgart Hytrulo With Enhanze for Subcutaneous Use in Generalized Myasthenia Gravis" (Press release). Halozyme Therapeutics. 20 June 2023. Archived from the original on 24 June 2023. Retrieved 24 June 2023 – via PR Newswire.
- ^ "Argenx Announces U.S. Food and Drug Administration Approval of Vyvgart Hytrulo (efgartigimod alfa and hyaluronidase-qvfc) Injection for Subcutaneous Use in Generalized Myasthenia Gravis". Argenx (Press release). 20 June 2023. Archived from the original on 24 June 2023. Retrieved 24 June 2023.
- ^ "Novel Drug Approvals for 2023". U.S. Food and Drug Administration (FDA). 28 June 2023. Archived from the original on 21 January 2023. Retrieved 28 June 2023.
- ^ "UCB announces U.S. FDA approval of Rystiggo (rozanolixizumab-noli) for the treatment of adults with generalized myasthenia gravis" (Press release). UCB. 27 June 2023. Archived from the original on 28 June 2023. Retrieved 28 June 2023 – via PR Newswire.
- ^ a b c Mehndiratta MM, Pandey S, Kuntzer T (October 2014). "Acetylcholinesterase inhibitor treatment for myasthenia gravis". The Cochrane Database of Systematic Reviews. 2014 (10): CD006986. doi:10.1002/14651858.CD006986.pub3. PMC 7390275. PMID 25310725.
- ^ "Atropine – Myasthenia-gravis medicines and drugs". NHS Choices. 2014. Archived from the original on 12 July 2015. Retrieved 11 July 2015.
- ^ a b c d e f g h Kumar V, Kaminski HJ (February 2011). "Treatment of myasthenia gravis". Current Neurology and Neuroscience Reports. 11 (1): 89–96. doi:10.1007/s11910-010-0151-1. PMID 20927659. S2CID 41052495.
- ^ Drachman DB, Adams RN, Hu R, Jones RJ, Brodsky RA (1 June 2008). "Rebooting the immune system with high-dose cyclophosphamide for treatment of refractory myasthenia gravis". Annals of the New York Academy of Sciences. 1132 (1): 305–314. Bibcode:2008NYASA1132..305D. doi:10.1196/annals.1405.033. PMC 3390145. PMID 18567882.
- ^ Suh J, Goldstein JM, Nowak RJ (June 2013). "Clinical characteristics of refractory myasthenia gravis patients". The Yale Journal of Biology and Medicine. 86 (2): 255–260. PMC 3670444. PMID 23766745.
- ^ Tandan R, Hehir MK, Waheed W, Howard DB (August 2017). "Rituximab treatment of myasthenia gravis: A systematic review". Muscle & Nerve. 56 (2): 185–196. doi:10.1002/mus.25597. PMID 28164324. S2CID 19504332.
- ^ Juel VC (March 2004). "Myasthenia gravis: management of myasthenic crisis and perioperative care". Seminars in Neurology. 24 (1): 75–81. doi:10.1055/s-2004-829595. PMID 15229794. S2CID 260320936.
- ^ Cea G, Benatar M, Verdugo RJ, Salinas RA (October 2013). "Thymectomy for non-thymomatous myasthenia gravis". The Cochrane Database of Systematic Reviews (10): CD008111. doi:10.1002/14651858.CD008111.pub2. PMID 24122674.
- ^ Wolfe GI, Kaminski HJ, Aban IB, Minisman G, Kuo HC, Marx A, et al. (August 2016). "Randomized Trial of Thymectomy in Myasthenia Gravis". The New England Journal of Medicine. 375 (6): 511–522. doi:10.1056/NEJMoa1602489. hdl:2318/1601939. PMC 5189669. PMID 27509100. (Erratum: doi:10.1056/NEJMx170003, PMID 28471717, Retraction Watch)
- ^ Cup EH, Pieterse AJ, Ten Broek-Pastoor JM, Munneke M, van Engelen BG, Hendricks HT, van der Wilt GJ, Oostendorp RA (November 2007). "Exercise therapy and other types of physical therapy for patients with neuromuscular diseases: a systematic review". Archives of Physical Medicine and Rehabilitation. 88 (11): 1452–1464. doi:10.1016/j.apmr.2007.07.024. PMID 17964887.
- ^ Mehrizi M, Pascuzzi RM (September 2014). "Complications of radiologic contrast in patients with myasthenia gravis". Muscle & Nerve. 50 (3): 443–4. doi:10.1002/mus.24254. PMID 24677227. S2CID 206295540.
- ^ Sieb JP (March 2014). "Myasthenia gravis: an update for the clinician". Clinical and Experimental Immunology. 175 (3): 408–418. doi:10.1111/cei.12217. PMC 3927901. PMID 24117026.
- ^ Cea G, Benatar M, Verdugo RJ, Salinas RA (October 2013). "Thymectomy for non-thymomatous myasthenia gravis". The Cochrane Database of Systematic Reviews (10): CD008111. doi:10.1002/14651858.CD008111.pub2. PMID 24122674.
- ^ Dresser, Laura; Wlodarski, Richard; Rezania, Kourosh; Soliven, Betty (21 May 2021). "Myasthenia Gravis: Epidemiology, Pathophysiology and Clinical Manifestations". Journal of Clinical Medicine. 10 (11): 2235. doi:10.3390/jcm10112235. ISSN 2077-0383. PMC 8196750. PMID 34064035.
- ^ Losen M, Martínez-Martínez P, Phernambucq M, Schuurman J, Parren PW, De Baets MH (2008). "Treatment of myasthenia gravis by preventing acetylcholine receptor modulation". Annals of the New York Academy of Sciences. 1132 (1): 174–179. Bibcode:2008NYASA1132..174L. doi:10.1196/annals.1405.034. PMID 18567867. S2CID 3206109.
- ^ Vrinten C, van der Zwaag AM, Weinreich SS, Scholten RJ, Verschuuren JJ (December 2014). "Ephedrine for myasthenia gravis, neonatal myasthenia and the congenital myasthenic syndromes". The Cochrane Database of Systematic Reviews. 2014 (12): CD010028. doi:10.1002/14651858.CD010028.pub2. PMC 7387729. PMID 25515947.
- ^ Steinbeck JA, Jaiswal MK, Calder EL, Kishinevsky S, Weishaupt A, Toyka KV, Goldstein PA, Studer L (January 2016). "Functional Connectivity under Optogenetic Control Allows Modeling of Human Neuromuscular Disease". Cell Stem Cell. 18 (1): 134–143. doi:10.1016/j.stem.2015.10.002. PMC 4707991. PMID 26549107.
Further reading
[edit]- Zhang Z, Guo J, Su G, Li J, Wu H, Xie X (17 November 2014). "Evaluation of the quality of guidelines for myasthenia gravis with the AGREE II instrument". PLOS ONE. 9 (11): e111796. Bibcode:2014PLoSO...9k1796Z. doi:10.1371/journal.pone.0111796. PMC 4234220. PMID 25402504.
- "Diagnostic: Myasthenia gravis". National Center for Biotechnology Information (NCBI). U.S. National Library of Medicine. Archived from the original on 10 December 2017. Retrieved 11 July 2015.