Seminiferous tubule
| Seminiferous tubule | |
|---|---|
 | |
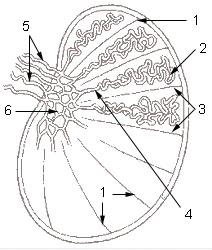 1: Testicular septa 2: Convoluted seminiferous tubules 3: Testicular lobules 4: Straight seminiferous tubules 5: Efferent ductules 6: Rete testis | |
| Details | |
| Identifiers | |
| Latin | tubuli seminiferi |
| MeSH | D012671 |
| TA98 | A09.3.01.022 |
| TA2 | 3599 |
| FMA | 19825 |
| Anatomical terminology | |
Seminiferous tubules (from Latin seminifer, meaning "seed-bearing") are highly convoluted tubes located within the testes where the process of spermatogenesis by meiosis occurs. These tubules are crucial for the production of spermatozoa, the male gametes essential for reproduction[1].
Structure
[edit]The epithelium of the tubule consists of a type of sustentacular cells known as Sertoli cells, which are tall, columnar type cells that line the tubule.
In between the Sertoli cells are spermatogenic cells, which differentiate through meiosis to sperm cells. Sertoli cells function to nourish the developing sperm cells. They secrete androgen-binding protein, a binding protein which increases the concentration of testosterone.
There are two types: convoluted and straight, convoluted toward the lateral side, and straight as the tubule comes medially to form ducts that will exit the testis.
The seminiferous tubules are formed from the testis cords that develop from the primitive gonadal cords, formed from the gonadal ridge.
Function
[edit]Spermatogenesis, the process for producing spermatozoa, takes place in the seminiferous tubules. During spermatogenesis, the DNA of spermatogenic cells in the seminiferous tubules is subject to damage from such sources as reactive oxygen species.[2] The genomic integrity of spermatogenic cells is protected by DNA repair processes. [3] Deficiencies in the enzymes employed in these repair processes may lead to infertility.[3]. The primary function of the seminiferous tubules is the production of spermatozoa through the intricate process of spermatogenesis. This complex biological process involves several stages of cell division and differentiation, ultimately leading to the formation of mature male gametes essential for fertilization[4].
Spermatogenesis
[edit]Spermatogenesis is the process by which spermatogonia, the primitive male germ cells, develop into fully mature spermatozoa. This process occurs within the seminiferous tubules and can be divided into three key phases:
- Mitotic Division: The process begins with spermatogonia, which are diploid cells situated at the basal layer of the seminiferous epithelium. These cells undergo several rounds of mitotic division to maintain the germ cell pool while also producing primary spermatocytes. This ensures a continuous supply of cells entering the subsequent stages of spermatogenesis[5].
- Meiotic Division: Primary spermatocytes, which are derived from spermatogonia, undergo the first meiotic division to produce two secondary spermatocytes, each containing half the number of chromosomes (haploid). These secondary spermatocytes quickly enter the second meiotic division, resulting in the formation of spermatids. During this stage, genetic recombination occurs, enhancing genetic diversity among the sperm cells[6].
- Spermiogenesis: Spermiogenesis is the final stage of spermatogenesis, where the round spermatids undergo a series of morphological and structural changes to become mature, motile spermatozoa. This involves the condensation of chromatin, the development of the acrosome (a cap-like structure that aids in fertilization), the formation of the flagellum (tail), and the shedding of excess cytoplasm[7].
Role of Sertoli Cells
[edit]Sertoli cells, which are also found within the seminiferous tubules, play a crucial supportive role in spermatogenesis. These somatic cells extend from the basement membrane to the lumen of the tubules and create a nurturing environment for the developing germ cells.
Additional images
[edit]-
Longitudinal section through the left side of the scrotum and the left testis (seminiferous tubules visible in center, but not labeled).
-
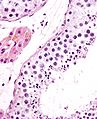
Seminiferous tubule (transverse section).
-
Photomicrograph of section through rat testis, showing seminiferous tubules.
See also
[edit]References
[edit]- ^ Alberts, Bruce (2015). Molecular Biology of the Cell (6th ed.). Garland Science. pp. 1128–1130. ISBN 978-0815344643.
- ^ Mahfouz R, Sharma R, Thiyagarajan A, Kale V, Gupta S, Sabanegh E, Agarwal A (2010). "Semen characteristics and sperm DNA fragmentation in infertile men with low and high levels of seminal reactive oxygen species". Fertil. Steril. 94 (6): 2141–6. doi:10.1016/j.fertnstert.2009.12.030. PMID 20117780.
- ^ a b Gunes S, Al-Sadaan M, Agarwal A (2015). "Spermatogenesis, DNA damage and DNA repair mechanisms in male infertility". Reprod. Biomed. Online. 31 (3): 309–19. doi:10.1016/j.rbmo.2015.06.010. PMID 26206278.
- ^ Clermont, Yves (2020). The cycle of the seminiferous epithelium in man. New York Academy of Sciences. pp. 281–293. ISBN 978-0897663674.
{{cite book}}: Check|isbn=value: checksum (help) - ^ de Rooij, Dirk G. (2018). "Proliferation and differentiation of spermatogonial stem cells". Reproduction. 156 (5): R155–R167. doi:10.1530/REP-17-0496.
- ^ Russell, L. David (2022). The Sertoli Cell. Springer. pp. 523–547. ISBN 978-1461492737.
{{cite book}}: Check|isbn=value: checksum (help) - ^ Fawcett, Don W. (2019). "The mammalian spermatozoon". Developmental Biology. 44 (3): 394–436. doi:10.1016/S0012-1606(71)80002-X.
External links
[edit]- Histology image: 17802loa – Histology Learning System at Boston University
- Image
- Diagram Archived 2007-02-19 at the Wayback Machine